Welcome to EHJ-ACVC Highlights, which spotlights articles from the European Heart Journal - Acute Cardiovascular Care that have recently captured the attention of the general cardiology community.
Delve into groundbreaking research and insights driving progress in acute cardiovascular and intensive care medicine.
Visuals credit: content is developed by Maria Bergami, Young ACVC Member, and the visual is created on Biorender.
We are proud to have had your attentive readership throughout this year and hope that this issue may again inform and inspire you. Here’s to a meaningful year ahead in acute cardiovascular care!
Enjoy!
Pascal Vranckx, David Morrow, Sean van Diepen, Frederik Verbrugge, editors.
For more updates and new groundbreaking science in area of #cvacute follow us on Social Media #EHJACVC @EHJACVCEiC
December 2025 Highlights
As the cold December days set in and the Holiday season begins, what better time to settle in with the latest issue of the European Heart Journal – Acute Cardiovascular Care? This December edition brings together an exceptional array of research spanning the full spectrum of acute cardiology and intensive care. With a special focus on thromboembolic disease, it builds on knowledge showcased in previous publications over the last two years that have explored right ventricular adaptation, advanced imaging, risk stratification, and mechanical circulatory support in pulmonary embolism.
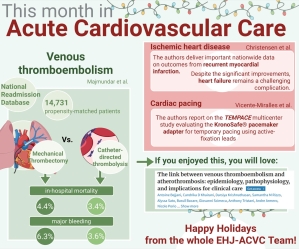
- Our December Editor’s Choice comes from Monil Majmundar, MD, and colleagues who analyzed 14,731 propensity-matched patients from the 2021 National Readmission Database to compare endovascular mechanical thrombectomy (MT) and catheter-directed thrombolysis (CDT) in pulmonary embolism. MT was associated with higher in-hospital mortality and major bleeding. Read more
- Among 24,799 patients in study performed in Denmark five-year mortality declined from 54.1% to 37.3%, heart failure hospitalizations from 13.6% to 11.7%, and subsequent recurrent MI from 23.4% to 17.7%. These improvements were consistent when stratified for age and sex, reflecting advances in pharmacologic and interventional management. Read more
- In the field of cardiac pacing, R. Vicente-Miralles, MD, and colleagues report on the TEMPACE multicenter study evaluating the KronoSafe® pacemaker adapter for temporary pacing using active-fixation leads in 30 patients. Only one minor complication occurred in the mean of 7.8 days, with stable electrical parameters and safe patient mobilization throughout. Particularly in TAVI patients, the system facilitated rhythm management and reduced unnecessary permanent pacemaker implantation. Read more
- Ji Hyun Cha, MD, and colleagues examined 878 patients with cardiogenic shock, distinguishing between isolated shock and mixed shock. Mixed cardiogenic shock affected nearly one-third of patients and was associated with markedly higher mortality, prolonged ventilation, and longer time to catheterization. Read more
- In a succinct yet impactful brief report, Sara Lozano-Jiménez, MD, and colleagues explore subclinical venous congestion in patients hospitalized for acute heart failure using VExUS. Despite appearing euvolemic at discharge, 24% of patients showed residual congestion—an independent predictor of adverse outcomes at six months highlighting the importance of imaging in optimizing treatment of these patients. Read more
- Finally, Antoine Bejjani, MD, and colleagues provide this month’s Educational Paper, highlighting the deeply interconnected nature of venous thromboembolism (VTE) and atherothrombosis. Read more
As we wrap up another remarkable year for EHJACVC, this December issue also stands to celebrate collaboration, curiosity, and clinical excellence. From groundbreaking research to thought-provoking reviews, every article reflects the dedication of our authors, the precision and passion of our reviewers, and the unwavering commitment of our editorial team. To you, our readers, we appreciate your engagement and enthusiasm which helps drive our mission forward.
November 2025 Highlights
November has come, with a new issue of EHJ–Acute Cardiovascular Care devoted to a formidable problem in medicine: acute myocardial infarction. Despite remarkable advances, MI still carries a heavy burden.
Together, these contributions are inspiring, highlighting actionable solutions that may improve patient outcomes at the bedside and strengthen cardiovascular care across health systems.
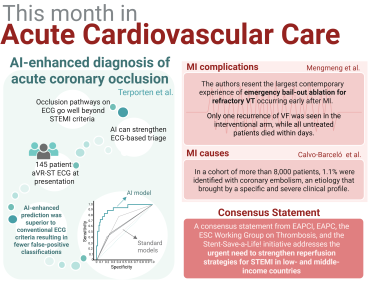
- Mengmeng Li and colleagues present the largest contemporary experience of emergency bail-out ablation for refractory VT, occurring early after MI. The results are striking, positioning ablation as a potentially life-saving option in situations where conventional measures fail. Read more
- Calvo-Barceló and collaborators shed light on coronary embolism as an underrecognized cause of MI. This study establishes coronary embolism as a distinct MI phenotype, with specific diagnostic and therapeutic challenges that require greater awareness. Read more
- In a research letter, Taggart and colleagues revisit type 2 myocardial infarction in older adults, showing higher five-year all-cause mortality compared with type 1 MI, though fewer deaths were cardiovascular in nature. Importantly, most subsequent cardiovascular events stem from atherosclerotic disease, underscoring the need for targeted prevention and intervention trials with cardiovascular-specific endpoints. Read more
- Johannes Terporten and colleagues present an elegant evaluation of AI-enhanced ECG interpretation for detecting acute coronary occlusion in patients with ST elevation in lead aVR. The findings suggest AI can meaningfully refine triage, reduce unnecessary angiography, and deliver faster, more accurate care in high-risk presentations. Read more
- Katia Orvin and colleagues provide new insights into the hemodynamic diversity of patients with high-degree atrioventricular (AV) block. This work highlights that AV block is not a uniform entity but encompasses distinct phenotypes with important implications for acute management and risk stratification. Read more
- Finally, a consensus statement from EAPCI, EAPC, the ESC Working Group on Thrombosis, and the Stent-Save-a-Life! initiative addresses the urgent need to strengthen reperfusion strategies for STEMI in low- and middle-income countries. (12) The document delivers practical recommendations across the care continuum, from early recognition to timely access to PCI, while acknowledging resource limitations and system barriers. Read more
September 2025 Highlights
As the vibrant city of Madrid wraps up another spectacular European Society of Cardiology (ESC) Scientific Sessions, the excitement is palpable — much like savoring a perfectly prepared jamón ibérico or a sizzling tapas spread after a long day. Just as Madrid’s culinary delights blend tradition with bold innovation, the latest research in acute cardiovascular and intensive care marries tried-and-true clinical wisdom with groundbreaking discoveries.
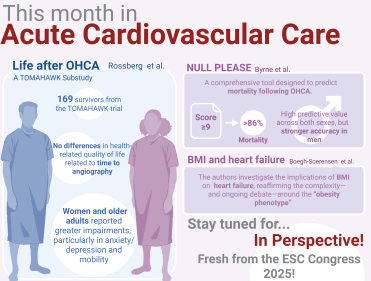
- Michelle Rossberg et al. report from the TOMAHAWK trial, exploring health-related quality of life (HRQoL) in 169 survivors of OHCA without ST-segment elevation. Notably, women and older adults reported greater impairments, particularly in anxiety/depression and mobility, underlining the importance of personalized post-arrest care. Read more
- Christina Byrne evaluates the NULL-PLEASE score, a comprehensive tool designed to predict mortality following OHCA. Validated using Danish nationwide data (n = 3,879), the score showed high predictive value across both sexes, but with stronger accuracy in men (AUCROC for 1-day mortality: 0.828 vs. 0.754; P < 0.001). For scores ≥9, one-day mortality exceeded 86%. The findings call for greater attention to sex-specific performance of risk models. Read more
- Sofie Boegh-Soerensen (3) investigates body mass index (BMI) and its implications in heart failure. Despite differences in cardiac structure and biomarkers, 6-month outcomes were similar across BMI groups, reaffirming the complexity—and ongoing debate—around the “obesity phenotype” in heart failure. Read more
- Julius Obergassel explores the detection of myocardial injury with three high-sensitivity cardiac troponin assays during left atrial ablation. The authors propose that this enhanced sensitivity may help clinicians distinguish acute from chronic myocardial injury with greater precision, particularly in patients with comorbidities like chronic kidney disease. Read more
Complementing these original contributions, we also open the door to 3 expert In Perspectives—a tasting menu of commentary blending sharp clinical insight with practical relevance to make complex science truly actionable. Fresh from ESC Congress 2025 in Madrid, this month’s feature highlights three groundbreaking late-breaking trials set to transform cardiology practice. DAPT-SHOCK-AMI, OPTION-STEMI, NEO-MINDSET
Together, this issue offers a rich banquet of evidence and insight — a true celebration of cardiovascular science at a moment when new discoveries promise to transform acute care.
August 2025 Highlights
As we open this issue of European Heart Journal – Acute Cardiovascular Care, we celebrate a landmark moment: the journal’s inaugural focus on paediatric acute cardiovascular and intensive care. This expansion reflects not only a growing scientific interest but a clinical imperative—children with acute cardiac illnesses demand specialised, evidence-driven strategies, and until now, their needs have been underrepresented in the acute cardiovascular literature. Our attention also turns to an increasingly important population: Grown-Up Congenital Heart Disease (GUCH), or ACHD (Adult Congenital Heart Disease) GRUNCH. Thanks to advances in pediatric cardiology and surgery, more patients with congenital heart disease now survive in adulthood, bringing with them complex anatomical and physiological challenges. These patients often present acutely, requiring an integration of congenital expertise with adult intensive cardiac care—a demand that is reshaping the landscape of emergency and critical cardiovascular services across Europe. Their inclusion as the journal’s editor’s choice this month is a natural extension of our commitment to comprehensive and inclusive acute cardiovascular care.
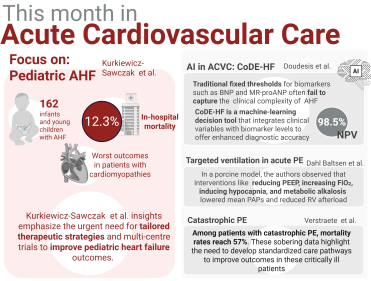
We are happy to host the retrospective cohort study by Kamila Kurkiewicz-Sawczak and colleagues, highlighting the complex and heterogeneous landscape of pediatric acute heart failure (AHF). Their study of 162 infants and young children—many just over a year old—reveals both the severity and the potential for improvement in this vulnerable group. 12.3% in-hospital mortality is a stark reminder of the stakes, while nearly 71% of patients showed significant echocardiographic improvement with appropriate care. Read more
This new paradigm is echoed in the work of Dimitrios Doudesis and colleagues (7), who introduce CoDE-HF, a machine learning–based decision-support tool for diagnosing acute heart failure. CoDE-HF integrates clinical variables with biomarker levels to offer enhanced diagnostic accuracy—classifying nearly half of patients as low-probability for AHF with a 98.5% negative predictive value. Read more
Tailoring therapy in a more wholistic framework is a theme carried on by Cecilie Dahl Baltsen and colleagues, who in an elegant porcine model, tested the hemodynamic effects of targeted ventilator settings in acute PE. Their randomized, controlled interventions—including reducing PEEP, increasing FiO₂, inducing hypocapnia, and metabolic alkalosis—all significantly lowered mean pulmonary artery pressure and reduced right ventricular afterload. Read more
Andreas Verstraete and colleagues reviewed 90 adult patients treated with advanced therapies including thrombolysis, surgical thrombectomy, and VA-ECMO. Among those classified as catastrophic PE—many presenting with cardiac arrest—the in-hospital mortality reached a staggering 57%. Notably, surgical thrombectomy was associated with significantly lower mortality (9%) compared to thrombolysis (49%), and major bleeding complications were confined to thrombolysis recipients. Read more
In closing, this issue of the European Heart Journal – Acute Cardiovascular Care reflects a field that is expanding—across the lifespan, across disciplines, and across frontiers of knowledge. From fragile pediatric hearts to adult patients with inherited cardiac legacies, from machine-enhanced diagnostics to precision ventilation strategies, we see a common thread: the need for rapid, tailored, and forward-looking interventions
July 2025 Highlights
Welcome to the July issue of the European Heart Journal – Acute Cardiovascular Care, in which we spotlight the evolving and high-stakes landscape of cardiogenic shock (CS). This lethal and complex syndrome is increasingly shaped by precision diagnostics and individualised therapies. Despite advances, complications like bleeding and acute kidney injury (AKI) continue to drive poor outcomes. As frontline teams face a continued drumbeat of acute myocardial infarction complicated by cardiogenic shock (AMI-CS), this issue highlights the critical role of individualised, physiology-based care, advanced diagnostics, and harm-reduction strategies — including optimal access site selection and antithrombotic use in improving survival.
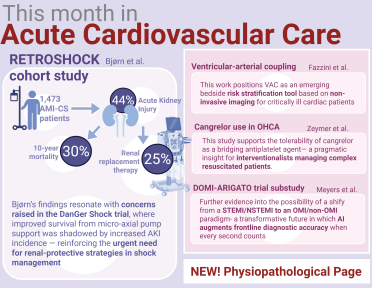
- The editor’s choice is the retrospective observational study by Dr. Bjørn using data from the Danish RETROSHOCK cohort. Among 1,473 patients, 44% developed AKI, with 25% requiring renal replacement therapy (RRT). Mortality was more than 30% higher at 10 years among those who developed AKI (p<0.001), positioning AKI as a major prognostic determinant in AMI-CS. Read more
- From the Mayo Clinic, Dr. Fazzini and colleagues contribute a powerful retrospective study assessing the prognostic utility of ventricular-arterial coupling (VAC) in 4,685 critically ill cardiac intensive care patients. Using a simple, non-invasive ratio (left ventricular end-systolic volume/stroke volume [LESV/SV]), the study demonstrates that a VAC ratio >2 was independently associated with increased in-hospital and 1-year mortality. Read more
- Dr. Zeymer and colleagues’ retrospective analysis of cangrelor use in patients with out-of-hospital cardiac arrest (OHCA) undergoing PCI. In a cohort of 414 patients, cangrelor was shown to provide potent platelet inhibition without increasing major bleeding risk, even in the high-risk subgroup treated with extracorporeal CPR. Read more
- In a clinically grounded and practical contribution, François Roubille and collegues present an educational review on the early management of acute myocarditis. Read more
- We are also proud to debut a new section: The Physiopathological Page. In this inaugural feature, Dr. Johannes Grand from Copenhagen University Hospital explores the metabolic signatures of cardiogenic shock, examining lactate dynamics and context-specific variations across shock phenotypes. Read more
As many of us approach a summer reprieve, this issue reminds us that even in the heat of July, the science of critical care never rests.
June 2025 Highlights
Cardiogenic shock (CS) remains one of the most critical and life-threatening conditions in acute cardiovascular care and presents clinicians with a formidable challenge. This complex syndrome, triggered by decompensation of chronic heart failure, acute myocardial infarction (AMI), or other cardiovascular insults, demands urgent and tailored interventions to enhance survival. Despite substantial advances in technology and pharmacotherapy, outcomes for these patients remain poor, particularly among those with complicating comorbidities such as cancer, liver dysfunction, and chronic respiratory diseases.
This issue focuses on research that is trying to take a step forward into improving outcomes of our patients.
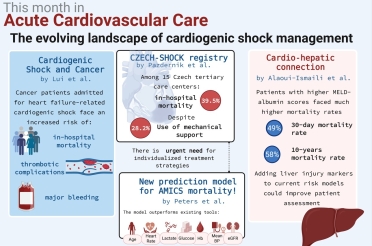
- An eye-opening study by dr. Liu et al. highlights the increased risks faced by cancer patients admitted for heart failure-related cardiogenic shock (HF-CS). Analyzing data from 137,316 admissions between 2014 and 2020, the research reveals critical differences in outcomes between cancer patients (n=7,306) and non-cancer patients. Cancer patients are at a significantly higher risk for in-hospital death, thrombotic complications, and major bleeding, with varying risks based on cancer type. Read more
- In the CZECH-SHOCK registry, Michal Pazdernik et al. (21) present a landmark national, prospective analysis of cardiogenic shock across 15 tertiary care centers in Czechia. Among 418 patients, the study reports a high 30-day mortality rate of 39.5%, despite mechanical circulatory support (MCS) use in 28.2% of cases. These findings underscore the urgent need for individualized treatment strategies and refined risk stratification in this critically ill population, providing crucial real-world data to guide future clinical trials and inform healthcare policy. Read more
- Aligning with this effort to improve cardiogenic shock management, Elma J. Peters et al. introduce a robust 30-day mortality prediction model for AMICS, developed from over 2,200 patients in the Netherlands and externally validated in Denmark. The model outperforms existing tools, offering clinicians a validated, rapid, and practical method for accurate risk assessment—essential for improving outcomes in AMICS. This rigorously developed and externally validated model is not only a leap forward in clinical decision-making but also an asset for quality assessment and patient selection in future trials. Read more
- Shifting focus to an often-overlooked factor in heart care, Zakaria Alaoui-Ismaili and colleagues bring a fresh perspective on the role of liver injury in cardiogenic shock outcomes. In their retrospective cohort study of 1,716 AMICS patients, they examined how liver dysfunction—measured using the MELD-albumin score—is associated with mortality rates. Read more
April 2025 Highlights
With the arrival of spring, the long-anticipated congress season is in full bloom, kicking off with the Acute Cardiovascular Care Congress in Florence, Italy. This vibrant gathering unites the global acute cardiovascular care community for an inspiring exchange of knowledge, groundbreaking research, and professional collaboration. But the momentum doesn’t stop there—April also brings the prestigious American College of Cardiology (ACC) Meeting in Chicago, where the European Heart Journal – Acute Cardiovascular Care takes center stage in capturing the latest scientific advancements. These landmark events offer an unparalleled platform for cutting-edge science, fostering collaborations, and exploring innovations shaping the future of cardiovascular medicine.
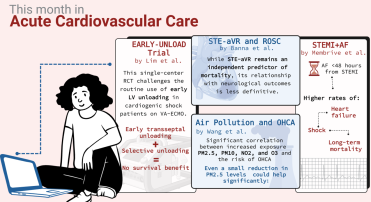
- Among the most compelling studies featured in this issue is the EARLY-UNLOAD trial by Yongwhan Lim et al. which examines the long-term impact of early left ventricular unloading in patients with cardiogenic shock undergoing circulatory support with veno-arterial extracorporeal membrane oxygenation (VA-ECMO). Read more
- Maria Jose Martinez Membrive’s research adds another dimension to our understanding of acute cardiovascular conditions by investigating the long-term prognosis of ST-elevation myocardial infarction patients complicated by atrial fibrillation. Read more
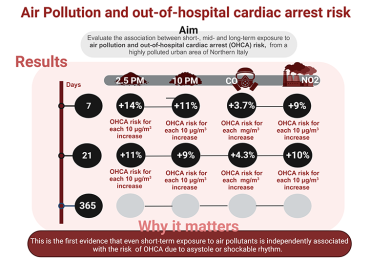
- Adding an environmental perspective to acute cardiovascular care, Jingjing Wang’s study examines the link between air pollution and out-of-hospital cardiac arrest (OHCA) in Shenzhen, China. This research underscores the profound impact of environmental factors on cardiovascular emergencies and highlights the importance of integrating pollution mitigation into cardiovascular prevention strategies. Read more
- Further deepening our understanding of post-cardiac arrest care, Soumya Banna’s study investigates the prognostic significance of ST-segment elevation in lead aVR (STE- aVR) in patients who achieved return of spontaneous circulation (ROSC) following cardiac arrest. Read more
- As the congress season unfolds, attention turns to the American College of Cardiology meeting in Chicago, where groundbreaking late-breaking trials are set to influence clinical practice. Among these, the ALT-SHOCK-2 trial will assess the effectiveness of early intra- aortic balloon pump placement in heart failure patients experiencing cardiogenic shock Meanwhile, advancements in deep learning for electrocardiogram-based risk stratification are poised to transform coronary revascularization decision-making in emergency departments Additionally, the RIVAWAR trial will compare the efficacy of rivaroxaban versus warfarin in patients with acute left ventricular thrombus following myocardial infarction, providing crucial insights into anticoagulation strategies.
- Beyond clinical trials, this issue also delves into the ethical complexities of end-of-life care in intensive therapy units, with JL Vincent offering a thought-provoking discussion on the principles guiding difficult decisions in the ICU. Read more
March 2025 Highlights
As cardiovascular care evolves at a rapid pace, so too does our understanding of the intricacies surrounding the diagnosis, treatment, and prognosis of patients with acute cardiovascular conditions. In the March issue of the European Heart Journal—Acute Cardiovascular Care, we delve into a collection of pivotal studies and expert perspectives that may help reshape our approach to managing acute myocardial infarction, myocardial injury, and chronic coronary syndromes.

- Boeddinghaus et al. present a groundbreaking prospective cohort study, offering a new classification system for Type 2 myocardial infarction based on cardiac imaging with coronary angiography and cardiac magnetic resonance imaging. This classification challenge s traditional diagnostic thresholds, separating out those without obstructive coronary disease or myocardial abnormality and seeking to provide clearer pathways to understanding the underlying pathology, with crucial implications for patient outcomes and preventive therapies. Read more
- In a different vein, Restan et al. offer an important validation study on the Siemens Atellica IM high-sensitivity cardiac troponin I assay. This study provides compelling evidence for the assay’s potential to optimize cardiac evaluations in emergency departments globally, bringing clarity to the decision-making process for patients presenting with non–ST-elevation MI. Their findings underscore the potential of rapid, high-sensitivity assays to transform acute care settings and improve patient outcomes. Read more
- Alaoui-Ismaili et al. investigate a niche but important intersection between post-cardiac neuroprognostication in AMICS patients supported by the Impella micro-axial flow pump, revealing the confounding impact of haemolysis on neuron-specific enolase levels. The study calls for caution in interpreting NSE levels, highlighting the complexity of prognostic markers in this patient population. Read more
- Additionally, our Perspectives section explores the 2024 European Society of Cardiology guidelines for chronic coronary syndromes, with an in-depth focus on ischaemia with non-obstructive coronary arteries and antithrombotic therapy, providing expert insights into these complex conditions.
Read more:
- Antithrombotic therapy in patients with chronic coronary syndrome: a focus on the 2024 European Society of Cardiology guidelines
- Ischaemia with non-obstructive coronary arteries in the 2024 European Society of Cardiology guidelines for the management of chronic coronary syndromes
- Hickman et al.’s educational paper critiques the evolving role of the 99th percentile in cardiac troponin assays, stressing the importance of context and understanding the limitations of this threshold in clinical decision-making. Read more
- Finally, Verbeeck et al. present a timely examination of the shift towards patient-centric outcomes in clinical trial design, advocating for the increasing importance of superiority trials over non-inferiority designs. This shift is exemplified by the REC-CAGEFREEI trial, which provides critical insights into how we assess and improve therapies aimed at enhancing patient safety and well-being. Read more
- We would like to take this opportunity and warmly invite you to explore the latest advancements in acute cardiovascular and intensive care at this year’s Annual Conference in Florence. Whether you are a clinician, researcher, or healthcare professional, this conference is an opportunity to stay at the forefront of your field and engage with peers who share your passion for improving patient outcomes. Follow us using an official hashtag #ACVC2025. See you in Florence !
Registration for the Acute Cardiovascular Care Congress
February 2025 Highlights
The February issue of the European Heart Journal Acute Cardiovascular Care highlights potentially groundbreaking translational research and clinical studies, showcasing innovations that may reshape acute cardiovascular medicine. From inflammation and diagnostic advancements to device innovation, this issue offers clinically impactful findings and expert commentary, affirming the journal’s leadership in bridging bench science and bedside care.

- A pivotal sub-study of the ECLS-SHOCK trial by Schupp et al. - a crucial role of inflammation in management of AMI-CS? Read more
- Honda et al. bring further translational insight with the LASCAR-AHF trial, evaluating low-dose carperitide (recombinant α-human A-type natriuretic peptide) in acute heart failure Rread more
- Optimizing mechanical support in cardiogenic shock - high vs low flow PVADs ? Observational study by Ikeda et al. utilizing Japanese PVAD registry Rread more
- Innovation at its glance - using arteficial intelligence in predicting AHF using data from around 19000 emergency room visits. Outstanding accuracy by external validation. A one big step forward in setting a new standard of precision medicine in emergency care. Read more
- Review by Van Aerde et al. underscores the importance of patient-centred models to improve long-term outcomes in CICU survivors focusing on weakness acquired in cardiac ICU Read more
- “Best of” series focuses this month on acute aortic syndromes highlighting the importance of this topic. Read more
- If you want to know more, deep dive into selected papers and read the issue summary prepared by our editors
Enjoy!
January 2025 Highlights
As we welcome 2025, the European Heart Journal – Acute Cardiovascular Care delivers a January issue that exemplifies the transformative spirit of innovation in our field. This first issue of the year sets the stage for progress by highlighting pivotal research featured in the journal in 2024 and forward-thinking ideas that promise to shape the future of acute cardiovascular and intensive care.
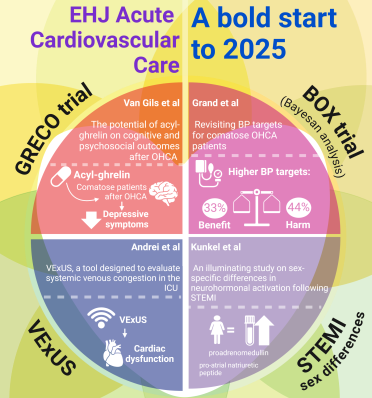
- Among the standout studies featured this month is the GRECO trial by Pauline C.W. van Gils et al., which explored the potential of acyl-ghrelin to improve cognitive and psychosocial outcomes following out-of-hospital cardiac arrest (OHCA). Findings in this trial, though preliminary, highlight the neuroprotective potential of acyl-ghrelin and call for further investigation into its broader role in post-cardiac arrest care. Read more
- Johannes Grand et al. provides a secondary Bayesian analysis of the BOX trial, revisiting blood pressure targets for comatose OHCA patients. Intriguingly, the analysis identified age-related differences, with younger patients showing increased mortality risks at higher MAP levels. These results underscore the complexity of post-resuscitation care and the need for personalized approaches tailored to individual patient profiles. Read more
- In another groundbreaking study, Stefan Andrei et al. critically examined the Venous Excess Ultrasound Grading System (VExUS), a tool designed to evaluate systemic venous congestion in the intensive care unit (ICU). Analyzing over 500 hemodynamic evaluations, the study found that higher VExUS grades correlated predominantly with cardiac dysfunction parameters, such as left ventricular E/A ratio and right ventricular S-wave velocity. However, the tool demonstrated limited utility in non-cardiac conditions like sepsis, emphasizing the need for complementary methods to assess congestion in diverse ICU populations. Read more
- Joakim Bo Kunkel et al. provide an illuminating study on sex-specific differences in neurohormonal activation following ST-elevation myocardial infarction (STEMI). Their multicenter investigation revealed that women exhibited significantly higher levels of biomarkers, such as pro-atrial natriuretic peptide and mid-regional proadrenomedullin, compared to men, alongside longer treatment delays and higher mortality rates. Read more
Complementing these original investigations is our signature “Best in the Year” series, which this month focuses on:
December 2024 Highlights
With warmth and excitement, we proudly present the final issue of European Heart Journal: Acute Cardiovascular Care in 2024! As the year closes, we’re excited to bring you a collection of thought-provoking and impactful articles — perfect reading for winter nights.
This issue features three groundbreaking research papers, two perspectives on leading-edge clinical trials, and an insightful educational piece on ethics in cardiac care research.
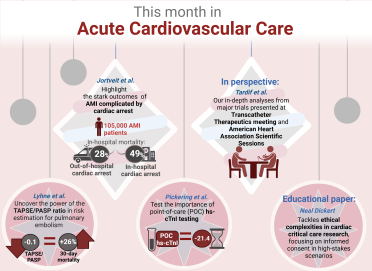
- Jarle Jortveit’s extensive Norwegian cohort study, highlights the stark outcomes for patients with acute myocardial infarction (AMI) complicated by either out-of-hospital (OHCA) or in-hospital cardiac arrest (IHCA). Analyzing over 105,000 AMI patients, the study found in-hospital mortality rates of 28% for OHCA and a striking 49% for IHCA. While survivors of OHCA achieved long-term survival comparable to those without cardiac arrest. In contrast, IHCA survivors continue to face elevated long-term mortality. These results emphasize the need for targeted interventions, particularly for IHCA patients who remain vulnerable post-discharge.
Read more - Our 2 Perspectives capture the latest exciting content from the prominent Autumn Cardiology conferences of 2024, including this year’s Transcatheter Therapeutics meeting in Washington and the American Heart Association Scientific Sessions in Chicago. Highlights include the SYNERGY (OASIS-9) trial, examining the impact of colchicine and spironolactone on post-AMI outcomes, and the GLORIUS trial, which contrasts oxygenation strategies during coronary and aortic surgeries. The former includes a trial interpretation from Dr. JC Tardif, principal investigator of the COLCOT trial, where he provides insights and interprets the data in the context of his own trial results.
Read more - Highly in the lineup, Mads Dam Lyhne’s study takes a closer look at the prognostic power of the Tricuspid Annular Plane Systolic Excursion/ Pulmonary Artery Systolic Pressure (TAPSE/PASP) ratio in evaluating patients with acute pulmonary embolism. Drawing from the extensive RIETE (Registro Informatizado de Enfermedad TromboEmbólica) registry data, this study spans 4,478 patients across European Society of Cardiology-defined risk groups. A decrease in TAPSE/PASP ratio emerged as a significant predictor of 30-day mortality, particularly in intermediate-high risk patients where rates escalated to 3.4%. Impressively, each 0.1 decrease in TAPSE/PASP ratio upped mortality odds by 26%. This finding confirms TAPSE/PASP as a valuable risk-stratification tool for clinical care, enabling safer decision-making on the need for hospitalization.
Read more - Also in this issue, John W. Pickering’s team brings a real-world evaluation of point-of-care (POC) high-sensitivity troponin I (hs-cTnI) testing. Implemented as the primary troponin assay in the emergency department (ED), POC hs-cTnI testing reduced patient length of stay by an average of 32 minutes, translating to 21.4 fewer patient-hours each day. With comparable safety outcomes to traditional methods, these findings highlight the promise of POC hs-cTnI in boosting ED efficiency and patient flow. This efficient approach could transform patient care by easing emergency department crowding without compromising safety.
Read more - Lastly, an educational piece by Neal Dickert tackles ethical complexities in cardiac critical care research, focusing on informed consent in high-stakes scenarios. Dickert’s review outlines practical strategies to respect patient autonomy while advancing urgently needed cardiac research, spotlighting scenarios where prospective consent may be waived responsibly.
Read more
November 2024 Highlights
Welcome to the November issue of the European Heart Journal Acute Cardiovascular Care! As we transition into the final months of the year, the days may be getting shorter, but the warmth in our field remains as we shine a spotlight on groundbreaking developments in cardiovascular care. This month’s edition brings a fresh perspective to some of the most pressing challenges in acute cardiovascular care, from innovative treatments for electrical storm (ES) to novel insights into the microcirculation in cardiogenic shock (CS). With each study, we edge closer to improving patient outcomes in life-threatening scenarios.
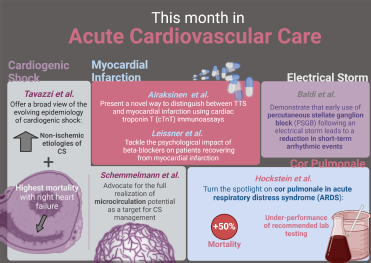
1. Enrico Baldi et al. demonstrated that the early use of percutaneous stellate ganglion block (PSGB) led to a dramatic reduction in arrhythmic events within the first hour, paving the way for safer, more effective interventions. PSGB offers new hope with potential to prevent progression to refractory ES—a breakthrough in an area where rapid intervention is critical. Although the study invites further exploration through randomized trials, the results are promising and may redefine how we approach ES in its early stage.
2. Maxwell Hockstein et al. shed the light into often-underdiagnosed condition of cor pulmonale in acute respiratory distress syndrome (ARDS). Their analysis reveals that cor pulmonale is associated with a 50% higher mortality rate, emphasizing the need for early identification. By examining factors such as pulmonary artery pulsatility index and arterial elastance (Ea), the study highlights that traditional metrics, including pH and PaO2, are less reliable predictors. This work stresses the necessity for multimodal diagnostics to better understand right ventricular-pulmonary artery coupling and prevent complications in ARDS—a call for greater awareness and proactive management.
3. Guido Tavazzi et al. offer a broad view of the evolving epidemiology of CS, examining data from over 11 000 ICU admissions in Italy. Their study reveals a shift from the traditional ischaemic causes to non-ischaemic etiologies and that right heart failure portends the highest mortality risk among CS patients. This trend potentially highlights the importance of early recognition and tailored interventions. As CS remains a condition with mortality rates hovering near 50%, this study underscores the need for integrated, multidisciplinary care strategies to improve survival outcomes.
4. On the front of mental health Leissner et al. tackle an often-overlooked consequence of cardiac care: the psychological impact of beta-blockers on patients recovering from myocardial infarction (MI). Drawing from the REDUCE-AMI trial, the authors found that while beta-blockers are associated with an increase in depressive symptoms, anxiety levels remain largely unaffected. Although the rise in depressive symptoms was modest, this finding reminds us of the importance of considering the mental health implications when managing MI patients, especially in those with preserved left ventricular ejection fraction. As we deepen our understanding of the interplay between cardiovascular and mental health, this study highlights the need for a holistic approach to cardiovascular patient care.
5. In a fascinating diagnostic advance, Juhani K.E. Airaksinen's study presents a novel way to distinguish between Takotsubo syndrome (TTS) and MI using cardiac troponin T (cTnT) immunoassays. The study’s discovery that TTS patients exhibit a significantly lower ratio of long to total cTnT compared to MI patients could offer a more precise diagnostic tool. While further research is needed to validate these findings with this investigational method, the potential for early differentiation between these two conditions could have a profound impact on treatment decisions, offering clinicians a powerful future tool in their diagnostic arsenal.
6. Rounding out this month’s issue is our educational paper from Christian Jung et al.9, which advocates for a more nuanced approach to CS management. By shifting focus from macrocirculation to microcirculatory dysfunction, this paper makes a compelling case for integrating microcirculation assessments into clinical practice. The authors emphasize that while advances in microcirculation-guided therapies hold great promise, their full potential has yet to be realized. More research is needed to bridge the gap between theoretical benefits and practical application in the ICU setting.
As we close this November issue, we invite our readers to engage with these pioneering studies, which collectively push the boundaries of cardiovascular care. We are excited about the discoveries shared in this edition, and we thank the authors for their invaluable contributions to our understanding of acute cardiovascular conditions. Together, let us continue to explore new horizons, expanding the possibilities of what can be achieved in the care of critically ill patients. Stay with us as we move into the final months of the year, energised, and optimistic about the future of our field.
October 2024 Highlights
In this month’s edition of the European Heart Journal - Acute Cardiovascular Care, we engage with some of the most critical issues facing contemporary acute cardiovascular medicine, including cardiogenic shock, out-of-hospital cardiac arrest, and the pressing need for sustainable practices in our healthcare systems. As we navigate these complex challenges, the insights shared by esteemed authors in this issue illuminate pathways towards improved patient outcomes and enhanced healthcare delivery. Enjoy!
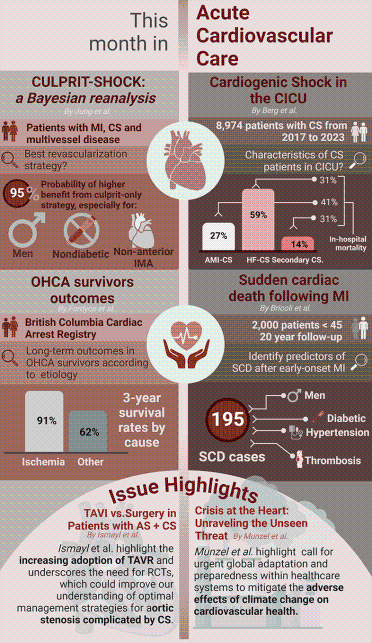
- Christian Jung contributes significantly to the discourse on acute myocardial infarction (AMI) and cardiogenic shock through his Bayesian reanalysis of the CULPRIT-SHOCK trial
This nuanced understanding underscores the necessity for personalized risk-benefit assessments in clinical practice, illustrating the value of Bayesian methods in interpreting complex trial data to enhance decision-making in high-risk populations.
Read more - The outcomes for survivors of out-of-hospital cardiac arrest (OHCA) are thoroughly explored by Christopher Fordyce et al who utilizes data from the British Columbia Cardiac Arrest Registry. Among 1,325 survivors, the study demonstrates that those with a reversible ischemic cause exhibit the highest three-year event-free survival rate of 91%, compared to only 62% for those with reversible non-ischemic causes. Conversely, heightened attention is warranted for patients with non-ischemic causes. Fordyce’s research not only sheds light on the long-term outcomes of OHCA survivors but also calls for a more refined approach to their management.
Read more - In a comprehensive analysis of the epidemiology of cardiogenic shock within a cardiac intensive care unit setting, David Berg et al utilizes the Shock Academic
Research Consortium (SHARC) definitions to classify distinct patient populations. Berg’s study highlights the utility of SHARC definitions in identifying distinct cardiogenic shock subpopulations with varying clinical outcomes, ultimately informing clinical practice and future research directions.
Read more - The risk of sudden cardiac death (SCD) following early-onset myocardial infarction (MI) is explored by Serena Bricoli who leverages a large cohort of 2,000 patients under the age of 45 and followed for a median of 19.9 years. Key independent predictors identified through multivariable analysis include diabetes, hypertension, previous thromboembolic events, a high Syntax score, and a lower left ventricular ejection fraction (LVEF) post-MI. Bricoli’s findings underscore the need for proactive monitoring and targeted interventions for individuals at risk.
Read more - At the forefront of this edition, Mahmoud Ismayl et al. present a nationwide study analyzing outcomes of 16,072 patients with aortic stenosis complicated by cardiogenic shock who underwent either transcatheter aortic valve replacement (TAVR) or surgical aortic valve replacement (SAVR) from 2016 to 2021. Ismayl’s study not only highlights the increasing adoption of TAVR but also underscores the need for randomized controlled studies, which could ultimately help to refine our understanding of optimal management strategies for these patients.
Read more - And last, but not least, explore this month’s statistical spotlight which delves into best practices and clinical guidance in extension studies for revascularization in left main coronary artery disease. Understanding the intricacies of statistical analysis not only enhances the quality of clinical research but also informs evidence-based practice, ultimately driving improvements in patient care.
Read more
September 2024 Highlights
Welcome to the September 2024 edition of the European Heart Journal - Acute Cardiovascular Care.
As the world revels in the afterglow of the spectacular 2024 Olympic Games in Paris, celebrating human endurance and triumph, we also mark the incredible breakthroughs presented at the 2024 European Society of Cardiology (ESC) congress in London. This issue of the European Heart Journal - Acute Cardiovascular Care (EHJ-ACVC) features major advancements and insights in cardiac care, echoing the Olympic spirit of striving for excellence.
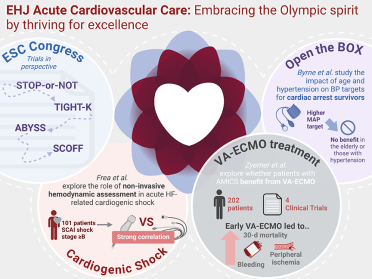
- STOP-or-NOT, TIGHT-K, ABYSS, SCOFF are the trials presented at 2024 ESC congress in London and in this issue are put in perspective due to its relevance to acute cardiac and intensive care medicine. These studies are investigating critical decision regarding the use of RAAS inhibitors, potassium supplementation in preventing atrial fibrillation post-cardiac surgery, the implication of beta blockers interruption in patient with history of myocardial infarction and last, but not least, fasting vs non-fasting before catheterization procedure.
- Frea et al. go one huge step forward exploring comprehensive non-invasive hemodynamic assessment in acute heart failure-related cardiogenic shock. They introduce a first prospective validation of echocardiographic estimation of PAPi, affirming its prognostic significance and advocation for broader use of echocardiography in assessing hemodynamics during HF-CS.
Read more
- In another pivotal study, sub-study of BOX trial Byrne et al. exlore the relevance of age and previous hypertension on MAP targets in comatose survivors of OHCA. The study showed that older patients and the ones with history of hypertension didn’t significantly benefit from a higher MAP target. Also, younger patients might have more benefit from lower MAP strategy, underscoring the need for personalized blood pressure management, particularly considering patient age.
Read more
- Finally, the manuscript by Uwe Zyemer et al. explores whether patients with infarct-related cardiogenic shock, like those in the Dan-Ger-Shock trial, benefit from VA-ECMO treatment. This individual patient data meta-analysis included 202 patients from four randomized clinical trials. Despite the study’s limited sample size, it provides the most comprehensive data to date on this topic.
Read more
August 2024 Highlights
This month, we spotlight pivotal research unveiling key insights into cardiogenic shock prognosis, personalised management of myocardial infarction, and innovative strategies in platelet inhibition.
As you prepare for THE cardiology event of the year this month in London, check the latest groundbreaking research that our editorial team prepared for you. Enjoy

- Rikken et al. present the evidence from On –TIME 2 trial demonstrating that prehospital tirofiban is independetly associated with higher risk of disrupted MI in STEMI pateints. This opens a new area for research in order to obtain inovative strategies of pre-hospital management for these patients.
Read more
- Samuel A. Watson et al.’s groundbreaking study introduces the validated CREST model, designed to predict circulatory etiology death (CED) following out-of-hospital cardiac arrest (OHCA). By comparing its efficacy with the SCAI shock classification, this study offers clinicians a refined tool for prognostication and therapeutic decision-making in OHCA, highlighting the potential to enhance patient selection for invasive interventions.
Read more
- Further enriching this issue, Siddharth M. Patel, MD, MPH, and Mathew S. Lopes, MD, MPH present pioneering insights into proteomic profiling of cardiogenic shock within the cardiac intensive care unit. Their study identifies nine biomarkers associated with CS, including sST2, FGF-23, CTSD, and GDF-15, thereby establishing a robust multi-marker model with diagnostic potential to facilitate early detection and personalized treatment strategies in critical care settings.
Read more
- Serena Bricoli and Giulia Magnani’s longitudinal cohort study on post-MI sudden cardiac death unveils a paradigm shift in risk stratification. (ref) By examining 2,000 young MI patients over two decades, their findings underscore the chronic nature of coronary atherosclerosis and emphasize tailored management strategies to mitigate traditional risk factors like diabetes and hypertension. This study, conducted in collaboration with leading European institutions, promises to reshape global prevention efforts and redefine clinical paradigms in cardiology.
5. Manning et al. introduce us into complexities of end-of-life care discussions within cardiac care units, unveiling evidence-based approaches to enhance shared decision-making for seriously ill older adults. Their insights offer structured frameworks to mitigate common pitfalls, ensuring patient-centered care aligns with individual values and preferences amidst the challenges of advanced heart disease.
Read more
July 2024 Highlights
Read this month's selection
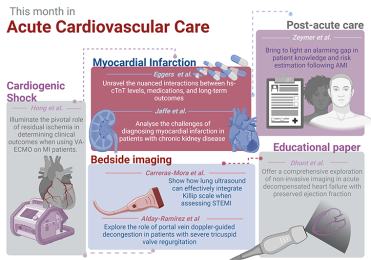
- Hong et al. present a study where they deal with the importance of residual ischaemia in AMICS undergoing VA-ECMO. In those cases residual ischaemia was associated with increased risk of 1-year mortality. However, further studies are needed to evaluate efficacy and future management of those patients.
- The correlation between hsTnT CV medications and long-term outcomes? – Can it have an effect on MAE?
- Elevated hs-cTnT levels pose a significant diagnostic hurdle, necessitating tailored diagnostic thresholds for accurate MI diagnosis in CKD patients. This study heralds a paradigm shift towards personalized diagnostic approaches to optimize patient care in this vulnerable population.
- Introduction of Killip pLUS scale– integration of Killip class and LUS provides better risk stratification than any of these used alone
- Portal vein dopler- the one and only that can track volume removal in severe TR. Further studies will provide answers if this strategy have a strong effect on patients outcomes.
- In GULLIVE-R prospective study the main focus is on secondary prevention strategies after AMI. Despite high adherence to guideline-recommended medications, only half of the patients receive all key secondary preventative medications, signaling a pressing need for enhanced education and prevention strategies.
- Finally, be prepared to dive deep into non-invasive imaging strategies in HFpEF, the educational paper prepared by Dhont et al. This article may provide you with resources you are looking for to provide your patients the best quality of care possible.
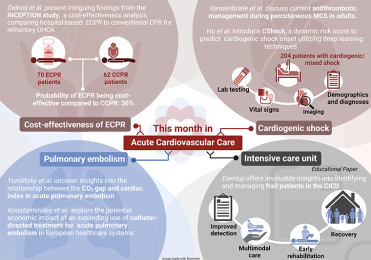
June 2024 Highlights
From the cost-effectiveness of eCPR, antithrombotic management during MCS and introduction of CShock score to predict cardiogenic shock onset by using AI, to contemporary management of pulmonary embolism and frail patients in ICU.
- Cost-effectiveness of extracorporeal cardiopulmonary resuscitation vs. conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a pre-planned, trial-based economic evaluation
- European practices on antithrombotic management during percutaneous mechanical circulatory support in adults: a survey if the Association for Acute CardioVascular Care of the ESC and the European branch of the Extracorporeal Life Support Organisation
- Developement and external validation of a dynamic risk score for early prediction of cardiogenic shock in cardiac intensive care units using machine learning
- Relationship between the mixed venous-to-arterial carbon dioxide gradient and the cardiac index in acute pulmonary embolism
- Modeling costs of interventional pulmonary embolism treatment: implications of US trends for a European healthcare system
- Frailty in the intensive care unit: assessment and impact
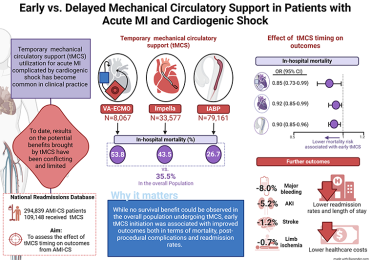
May 2024 Highlights
What is the best time for tMCS in AMI-CS - earlier the better?
Buda et al. conducted a study comparing early vs. delayed initiation of MCS in AMI-CS. Their findings suggest that early initiation of tMCS is associated with fewer adverse events, lower mortality and fewer readmissions compared to delayed tMCS.
Future prospective randomised studies are needed to identify patients who would benefit the most from tMCS and to select the adequate type of tMCS for each patient.
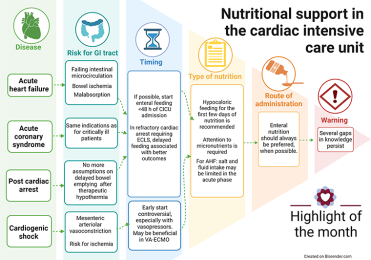
April 2024 Highlights
Nutritional support during ICU stay - a stepwise approach towards better outcomes
Nutritional support plays an important role in management of critically ill patients, especially patients with acute heart failure, acute coronary syndrome, post-cardiac-arrest patients and patients with cardiogenic shock.
Nutritional support in acute heart failure
The nutritional risk and prevalence of malnutrition is high in patients with acute heart failure (up to 40%) due to bowel ischemia, microcirculatory failure, and malabsorption. Although adequate nutrition might play an important role in improving outcomes, studies on this matter are still lacking.
Nutritional support for these patients is based on general principles- early nutritional assessment, form of administration and assessment of nutritional risk. It is recommended to start enteral feeding in the first 48h upon CICU admission. In the acute phase (<72h) it is best to implement hypocaloric nutrition with adequate substitution of micronutrients.
Parenteral feeding can be associated with higher risk of infection, and it is recommended as first line in case of severe gastrointestinal dysfunction. However, early parenteral feeding is recommended in severely malnourished patients.
Nutritional support in acute coronary syndrome
Malnutrition is these patients may be associated with worsening outcomes. The same principles apply as for critically ill patients.
Nutritional support after cardiac arrest
Patients after suffering cardiac arrest may require close monitoring, especially if receiving ECLS for refractory cardiac arrest. In those patients’ enteral nutrition should be introduced with caution, as rates of intestinal ischemia are higher. Delayed feeding is associated with better outcomes. Studies on this field are needed to create uniform protocols of management of these patients.
Nutritional support in cardiogenic shock
As we all know, cardiogenic shock is a low cardiac output state secondary to cardiac dysfunction, leading to end-organ hypoperfusion and tissue hypoxia. During this condition mesenteric arteriolar vasoconstriction plays a major role in trying to maintain systemic blood pressure. Together with venous congestion it leads to decrease in local perfusion and increased risk of bowel ischemia.
If enteral feeding is started in this highly vulnerable hemodynamic state, there is a risk of mesenteric ischemia. Starting early enteral feeding is still controversial. It may be beneficial to do a permissive underfeeding in the first few days, especially in patients who require use of vasopressors. The incidence of proven bowel ischemia using those protocols was <1%.
Having in mind the incidence and severity of cardiovascular diseases requiring CICU admission, comprehensive multidisciplinary approach to nutritional support is needed to optimize care of critically ill patients. Further research is needed to try to obtain uniform and individualized protocols that could improve patient survival, duration of ICU stay and quality of life after CICU admission.
March 2024 Highlights
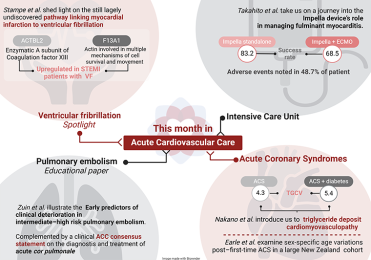
The light in the end of the tunnel – unrevealing mechanisms of ventricular fibrillation during the first ST elevation myocardial infarction by the use of proteonomics.
Stampe et al. conducted a study using proteonomics that unrevealed that 26 proteins are associated with ventricular fibrillation. Pending further analysis two of the proteins were strongly associated with VF (ACTBL2, F13A1). The findings of this study represent a groundbreaking moment that points the light towards further investigation of early VF in ST elevation myocardial infarction.
Embrace the challenge – the role of ventricular assist device in management of fulminant myocarditis
The study by Takahito Nasu et al. represent a pioneering large-scale registry study using data from Japanese Registry for Percutaneous Ventricular Assist Devices. Use of Impella device showed better success rate in comparison with ECPELLA. Having in mind the high percentage of adverse events further investigation is needed to optimize patient selection and treatment in this matter.
Deep dive into pulmonary embolism – identifying early predictors affects the outcome?
Zuin et al. deal with “Early predictors of clinical deterioration in intermediate-high risk pulmonary embolism” Their educational paper is complemented by a clinical consensus statement from the Association for Acute Cardiovascular Care that outlines the diagnostic and treatment pathways for acute right ventricular failure secondary to acutely increased right ventricular afterload.
Triglyceride deposit cardiomyovasculopathy (TGCV) – rare or just undiagnosed condition?
Nakano et al. introduce us to TGCV by conducting a study on 400 patients with ACS and 148 patients with diabetes and ACS. The study reports 4.3-5.4% prevalence emphasizing the need for further investigation and risk stratification of these patients, having in mind that they may present with diffuse coronary artery stenosis.
February 2024 Highlights
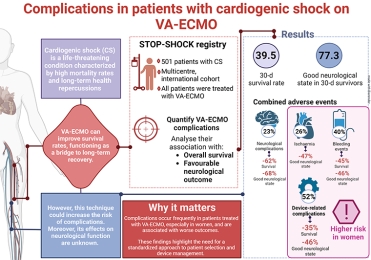
Cardiogenic shock patients on VA-ECMO – individual approach as the solution in prediction and reduction of complications?
VA-ECMO is a well-established method of treating patients with cardiogenic shock. But the risk of complications is still very high. Benedict N. Beer et al. conducted a retrospective multicenter cohort study with the aim to accurately describe the risk of complications and mortality events and to evaluate possible predictors of such events in those patients.
The study showed that the majority of 30-day survival patients treated with VA-ECMO had favorable neurological outcome (CPC 1/2). The presence of AEs, which are more common in women, are strongly associated with worsened neurological outcome and 30-day survival.
Further studies are needed to identify patients that could benefit from this strategy, having in mind the high risk of complications, whose prediction is still challeging and in need for RCTs. One possible solution might be the use of ECMELLA strategy that may reduce typical VA-ECMO complications but the strong evidence is still lacking. Patient selection might be improved by forming the multidisciplinary cardiogenic shock teams worldwide.
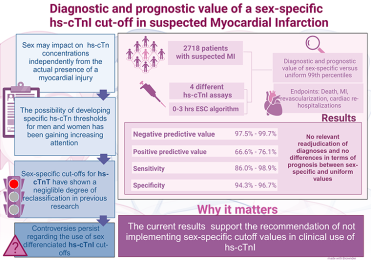
January 2024 Highlights
Sex-specific 99th percentile high-sensitivity cardiac troponin assays – are we there yet?
Dr. Maria Rubini Gimenez discusses the diagnostic and prognostic value of sex-specific 99th percentiles in high sensitivity cardiac troponin assays for AMI.
The study by Lehmacher et al. reveals comparable diagnostic accuracy between uniform and sex-specific cutoffs, suggesting no clear advantage for the latter.
The results extend this message to uniform cutoffs for hs-cTnI, but the diagnostic accuracy’s reliance on hs-cTnT concentrations is acknowledged as a limitation which requires futher studies before recommending sex-specific cutoffs in clinical practice.
Climate change as a global health problem – are we too late to prevent the consequences?
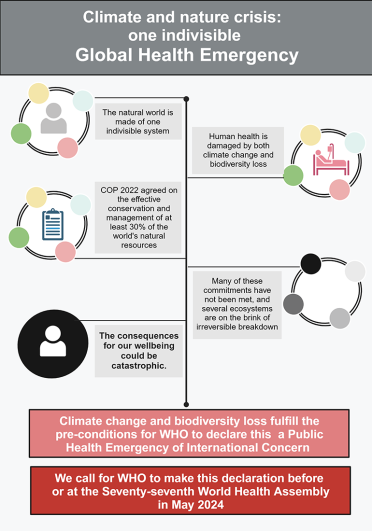
The EHJ-ACVC joins over 200 heart journals and urges the United Nations, political leaders, and health professionals to address climate change and biodiversity loss together as an indivisible global health emergency.
Recognising the interconnectedness of climate and nature crisis, they emphasise the severe impact on health, from infectious diseases to mental health issues. The call urges the WHO to declare this crisis a global health emergency to be able to restore biodiversity and combat climate change.
Figures from Maria Bergami

 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.