Take-home messages
- We must consider air pollution as another cardiovascular risk factor
- The participation of health professionals in risk reduction strategies associated with air pollution is necessary
Epidemiology
Air pollution is contamination of the indoor or outdoor environment by any chemical, physical or biological agent that modifies the natural characteristics of the atmosphere. According to WHO data, almost the entire global population (99%) is exposed to air pollution levels that are higher than recommended levels [1].
Air pollution is the known cause of over three million deaths every year due to ischaemic heart disease or stroke which is more than traditional cardiac risk factors such as diabetes, smoking or obesity. Air pollution is also the cause behind the 3% global-disability-adjusted life years [2]. Table 1 shows the main risk factors of global mortality, in order of relevance, with air pollution occupying one of the top places [3].
Table 1. Global mortality risk factors.
Modified from Brauer et al. Taking a Stand Against Air Pollution – The Impact on Cardiovascular Disease. A Joint Opinion from the World Heart Federation, American College of Cardiology, American Heart Association, and the European Society of Cardiology. Eur Heart J. 2021;42:1460-3. [3] with permission by Oxford University Press on behalf of the European Society of Cardiology.
| RANKING | RISK FACTOR | |
| 1 | Hypertension | |
| 2 | Smoking | |
| 3 | Unhealthy diet | |
| 4 | AIR POLLUTION | ENVIRONMENTAL |
| 5 | Diabetes | |
| 6 | Obesity | |
| 7 | Hyperlipidaemia | |
| 8 | Renal disfunction | |
| 9 | Malnutrition | |
| 10 | Alcoholism | |
| 11 | Temperature (non-optimal) | ENVIRONMENTAL |
| 12 | Unsafe water | ENVIRONMENTAL |
Air pollution includes particulate matter (PM), carbon monoxide (CO), ozone (O3), nitrogen dioxide (NO2) and sulphur dioxide (SO2). PM - inhalable particles - varies in composition and size and is usually classified into 3 size groups: coarse particles (PM10, diameter <10 and ≥2.5 μm), fine particles (PM2.5, diameter <2.5 μm), and ultrafine particles (<0.1 μm). PM2.5 (a well-documented health risk) originates from combustion and non-combustion sources including industrial emissions, brake and tire wear, resuspended soil and dust, wildfires and prescribed burns, and the burning of agricultural products, biomass and coal. The chemical constituents of PM2.5 vary by emission source and include elemental carbon, transition metals, complex organic molecules, sulphates, nitrates, soil, and dust. PM is capable of penetrating deep into the lungs and enters the bloodstream, impacting the cardiovascular (ischaemic heart disease), cerebrovascular (stroke) and respiratory systems. Both long- and short-term exposure to particulate matter is associated with morbidity and mortality from cardiovascular and respiratory diseases [4-5].
The latest WHO Air Quality Guidelines (2021) recommend the following concentration limits for these pollutants:
- PM2.5: Annual average 5 µg/m3; 24-hour average 15 µg/m3
- PM10: Annual average 15 µg/m3; 24-hour average 45 µg/m3
- NO2: Annual average 10 µg/m3; 24-hour average 25 µg/m3
These limits are vastly exceeded worldwide [1]. There are data as worrying as that a non-smoker living in New Delhi has the same cardiovascular risk as if he smoked 40 cigarettes a day.
But of course, this bad news is not new. Almost three decades ago, the New England Journal of Medicine published a study performed in six American cities in which the association of air pollution (mainly fine particles) with mortality was demonstrated, not only through lung cancer but in cardiovascular diseases as well [6]. In the same journal, many years later, we find a similar study, now carried out in 652 cities in 24 countries or regions across the globe, that showed independent associations between short-term exposures to PM10 and PM2.5 and daily all-cause, cardiovascular and respiratory mortality [7].
Twenty years ago, there was an editorial in Circulation on this topic titled “Air Pollution: An Insidious and Pervasive Component of Cardiac Risk” [8] and since then, not only the WHO but also the main scientific societies have written multiple statements on air pollution and cardiovascular disease [4,9]. The 2021 Clinical Practice Guidelines of the ESC on Cardiovascular Prevention [10] included a specific section on air pollution, and the same year the World Heart Federation, the American College of Cardiology, the American Heart Association, and the European Society of Cardiology published a joint opinion in an article called “Taking a Stand Against Air Pollution—The Impact on Cardiovascular Disease” [3].
Pathophysiology and clinical implications
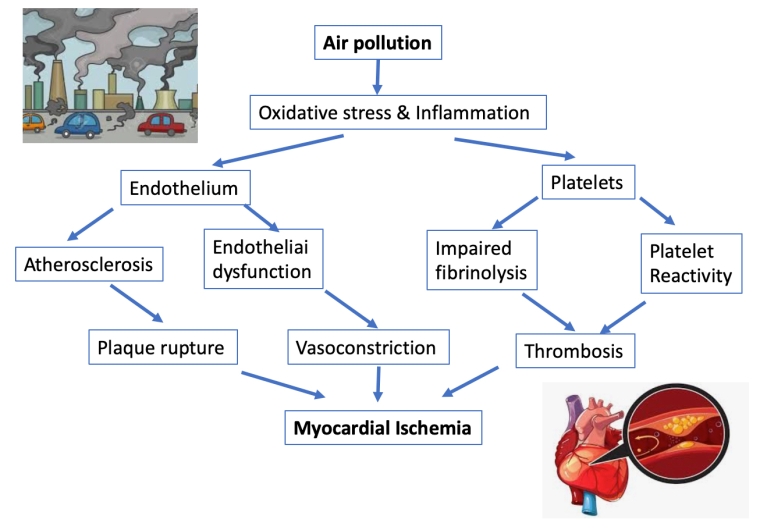
Several mechanisms related to air pollution are involved in cardiovascular disease, mainly the risk of atherothrombosis [5,11]. Some studies suggest that exposure to air pollution may increase blood pressure, exacerbate myocardial ischaemia, and trigger myocardial infarction. Many of these effects may be mediated through direct or indirect effects on the systemic vasculature, driven by endothelial dysfunction. In the European expert position paper on air pollution and cardiovascular disease, published in 2015 [4], the authors state the following (Figure 1):
“Exposure to PM2.5 potentiates plaque burden and vascular dysfunction in models of atherosclerosis, and is also associated with plaque vulnerability, alterations in vasomotor tone, increased reactive oxygen species and pro-inflammatory mediators. Oxidative stress is pro-inflammatory and conversely, inflammation is pro-oxidative, leading to a vicious cycle that results in high levels of oxidative stress. Systemic inflammatory effects of cytokines or oxidising molecules emanating from the lungs may also affect atherosclerotic plaques, leading to their progression, destabilisation, or rupture, precipitating acute coronary syndrome”.
There are also short-term associations between air pollution and cardiovascular mortality that can be explained by thrombogenicity; this is one of the reasons that acute coronary syndromes are linked to exposure to traffic. A relationship has been described between air pollution and traditional cardiovascular risk factors. Obese and diabetic people may be at higher risk of the cardiovascular effects of PM2.5 and conversely, long-term PM2.5 exposure may promote the development of overt diabetes mellitus, potentially through systemic inflammatory responses.
Figure 1. Possible mechanistic effects of air pollution on myocardial ischemia. Modified from Newby D et al. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36:83-93. https://academic.oup.com/eurheartj/article/36/2/83/2293343 [4] with permission by Oxford University Press on behalf of the European Society of Cardiology.
Observational studies in different populations have demonstrated acceleration of atherosclerosis. For example, in the participants of the Multi-Ethnic Study of Atherosclerosis and Air Pollution (MESA Air) study, increased concentrations of PM2·5 and traffic-related air pollution within metropolitan areas, in ranges commonly encountered worldwide, were associated with progression in coronary calcification [12]. In the Aragon Workers Health Study (AWHS), the association of a panel of toxic metals (the sum of inorganic arsenic, barium, cadmium, chromium, antimony, titanium, uranium, vanadium, and tungsten) measured in urine, was compared with a comprehensive panel of subclinical atherosclerosis, including atherosclerosis presence in the carotid, femoral, and coronary territories. The results were that arsenic, cadmium, and titanium exposures were positively associated with the presence of subclinical atherosclerosis, mainly driven by arsenic and cadmium in the carotid, cadmium and titanium in the femoral, and titanium in coronary territories [13].
Regarding the acute effects of air pollution, we have evidence such as the results of the Codi IAM registry in Spain, an article by Bañeras et al from the International Journal of Cardiology noted that “where short-term exposure to high levels of PM2.5 and PM10 was associated with increased daily STEMI admissions and STEMI-related ventricular arrhythmias and mortality: exposure to high levels of lead and NO2 was associated with increased daily STEMI admissions, and NO2 with higher mortality in STEMI patients” [14]. The worse prognosis of these patients could be related to a pro-inflammatory status. Another ongoing study in these patients is evaluating the influence of air pollution on the results of cardiac rehabilitation programs.
There is no doubt that the fundamental approach to this problem is prevention, but we also must consider interesting therapeutic proposals to combat some of the serious consequences of air pollution in cardiovascular disease. To this end, there is a research program on ethylene diamine tetra-acetic acid (EDTA) chelation, which has shown to be effective in removing metals such as cadmium and lead from the body. The Trial to Assess Chelation Therapy (TACT) study [15] included 1,708 participants >50 years old with previous acute myocardial infarction (>6 weeks before) and serum creatinine levels <2 mg/dl. The primary endpoint for the study was a composite of all-cause mortality, myocardial infarction, stroke, coronary revascularisation, or hospitalisation for angina. Disodium EDTA chelation reduced the primary composite endpoint by 18% (hazard ratio [HR]: 0.82; 95% confidence interval [CI]: 0.69-0.99; p<0.035). The number needed to treat (NNT) to prevent 1 event over 5 years of follow-up was 18. A total of 633 TACT participants (37%) had diabetes, a prespecified subgroup, in whom the reduction of the relative risk of the primary endpoint was 41% (HR: 0.59; 95% CI: 0.44-0.79; p<0.0002) over 5 years; in them the NNT to prevent 1 event over 5 years of follow-up was 6.5. [16].
A recent systematic review on “Chelation Therapy in Patients With Cardiovascular Disease”, included 4 clinical trials, 15 prospective before/after studies, and 5 retrospective case series assessing mortality, disease severity, plasma biomarkers of disease chronicity, and/or quality of life. The authors conclude that there are signs of benefits for EDTA in patients with atherosclerotic vascular disease and that patients with diabetes and peripheral artery disease may benefit more from EDTA therapy than other patient populations. It may be that EDTA eliminates toxic metals associated with atherosclerotic and oxidative vascular damage [17].
In a couple of years, a new study, TACT2, may provide definitive evidence of the benefits of edetate disodium-based chelation on cardiovascular outcomes, as well as the clinical importance of longitudinal changes in toxic metal levels of participants [18].
Time to act
Most professionals dedicated to cardiovascular health and disease have never worried about air pollution. This is perhaps due to ignorance, a feeling that the impact of air pollution exceeds our scope of action or to a lack of resources. However, for many years there has been a continually growing body of evidence making the link between air pollution and cardiovascular health increasingly clear. With this realization, we have seen more and more concern in public administrations, scientific societies and in the general population, so it is equally important that we incorporate this fact into our clinical practice. We must ask our patients about the environment in which they live, both outdoors and indoors, their place of work, etc. These factors are frequently related to socioeconomic levels and this information should be integrated into the estimation of cardiovascular risk and probably into the residual risk.
Of course, it is difficult improve situations at the individual level, so initiatives such as the recently created working group in Spain are necessary.
The Spanish Society of Cardiology (SEC) together with the Spanish Heart Foundation (FEC) has created the “SEC-FEC-Verde” Working Group (the Green SEC-FEC). The general objective of the project is to reduce the morbidity and mortality of cardiovascular diseases related to pollution.
The new working group of the Spanish Society of Cardiology and the Spanish Heart Foundation was born with the following objectives:
- Aid in the dissemination of knowledge of environmental pollutants (air pollution and metals, among others) as cardiovascular risk factors.
- Promote research in the field of environmental pollutants among the members of the SEC and participate in studies with other societies that are also interested in prevention in this field.
- Urge the SEC and the FEC to participate in prevention strategies in public health, to collaborate in the development of population measures and guidelines for cardiovascular prevention.
- Modify attitudes and use of materials or media in our society to act in accordance with preventive recommendations in this field.
- Create awareness among our partners of the importance of environmental contaminants in cardiovascular prevention, at the same level as other well-known and accepted risk factors in clinical management.
- Promote the creation of heart-healthy cities.
- Promote sustainable architecture environments
Conclusions
- Air pollution in not a new, but an ignored cardiovascular risk factor
- There is enough evidence on chronic and acute cardiovascular damage caused by air pollution
- The main scientific societies have published recommendations to reduce the negative consequences
- Clinicians cannot refrain from our obligation in cardiovascular prevention, which also includes aspects related to air pollution.
- In addition to global programs, local initiatives are necessary that include the general population.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.