Introduction
Transthoracic echocardiography (TTE) and, in a small number of patients, transoesophageal echocardiography (TEE) are important tools in aortic stenosis (AS) and aortic regurgitation (AR) which can provide information on the type and degree of valve dysfunction as well as on the haemodynamic burden induced by the valve defect in order to optimise diagnosis, stratify prognosis, and address management [1].
Aortic Valve Stenosis
Table 1. Measures of AS Severity.

N: number of instantaneous measurements
Transvalvular peak velocities (Vmax) and mean pressure gradients (ΔPmean) are needed to estimate the degree of stenosis [2]. Accurate recording of data involves the evaluation of all acoustic windows including the suprasternal and right parasternal windows for determining the highest velocities. The right parasternal window is often the location of the highest peak jet velocity if the left ventricular-aortic root angle is acute [3]. Averaging of at least five consecutive beats is recommended in patients with arrhythmia, avoiding measurements after postextrasystolic beats. If Vmax measured at the level of the left ventricular outflow tract (LVOT) is >1 m/s, ΔPmean AS has to be calculated by the modified Bernoulli equation and not by the simplified one. Whenever possible, the third essential parameter considered as appropriate is the evaluation of aortic valve area by continuity equation (AVAeff): it is needed since loading conditions influence transvalvular velocity and pressure gradient. AVAeff requires the cross-sectional area of the LVOT (CSALVOT) and LVOT flow velocity data, along with aortic velocity. The current standard approach used to estimate the CSALVOT is based on LVOT diameter measurements. It is a crucial estimation since: 1) two-dimensional (2D) measurement of diameter has to be performed accurately, by the TEE approach, because even a 1 mm difference can cause a 10% variation of left ventricular stroke volume (LVSV); 2) in some patients the diameter results in an underestimation of the normally oval-shaped CSALVOT. Three-dimensional (3D) echocardiography may provide an accurate assessment, thus avoiding underestimation due to geometric circular assumption, although a lower spatial resolution compared with 2D images and the level of expertise of individual operators have to be taken into account. A new concept of “hybrid imaging” can combine CSALVOT measured by contrast-enhanced multislice computed tomography with flow velocities measured by echo Doppler [4,5].
Aortic stenosis jet and LVOT velocity measurements have a very low intra- and inter-observer variability (3-4%) both for data recording and measurement in an experienced laboratory. However, the measurement variability for LVOT diameter ranges from 5 to 8%.
Additional parameters are the simplified continuity equation area (peak velocity instead of velocity-time integral), velocity ratio (the best to avoid an error in CSALVOT), and planimetry of the anatomic valve area (AVAgeom). TEE should be used for reliable measurement of AVAgeom and for a more accurate calcium estimation. Echocardiography is also a key tool for detecting secondary cardiac alterations typically caused by severe AS such as concentric LV hypertrophy, diastolic dysfunction and pulmonary hypertension.
Aortic stenosis is still a diagnostic problem: the main challenge for echocardiographers is to detect a possible misinterpretation [6]. In clinical practice in a small but not negligible proportion of patients, the necessity to characterise different AS scenarios has led to classification according to normal or low-flow conditions as well as high or low gradients. Generally, an underestimation of AS severity by determining velocity and gradients may occur during low-flow conditions, reduced LVSV and reduced LV function; on the other hand, an overestimation of severity may occur during hyperdynamic circulatory states (concomitant aortic regurgitation, anaemia, hyperthyreosis, etc.) and by pressure recovery when the aortic root is small (diameter of sinotubular junction <30 mm). Almost half of patients classified as having severe AS were reclassified as having non-severe AS when pressure recovery was taken into account [7].
Normal flow-low gradient AS with preserved or normal LV ejection fraction is described in the literature as a true entity. However, in clinical practice it can be assumed that most AS patients described as having these cardiac characteristics are misclassified by measurement errors due to overestimation of AS severity determining AVAeff by the continuity equation.
In addition, for diagnostic purposes, it seems to be useful to focus on prognostically relevant echocardiographic parameters in AS patients: a rapid progression of aortic jet velocities, low-flow low-gradient conditions, and LV global longitudinal strain, especially in the presence of a normal ejection fraction.
Aortic Valve Regurgitation
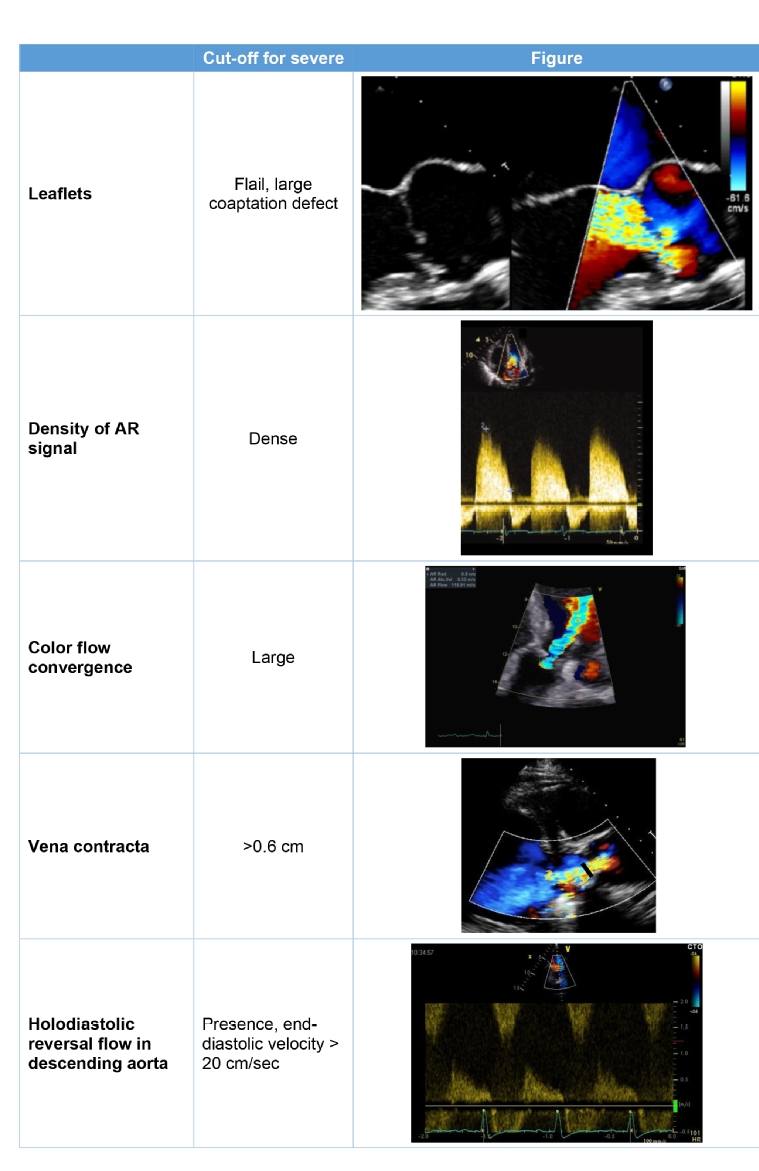
Table 2. Most Used Measures of AR Severity.
Unlike AS, the assessment of valve morphology, and the evaluation of mechanisms as well as careful measurement of the different segments of the aorta are more important in AR. TEE improves on the diagnostic accuracy of TTE by precisely defining the mechanisms, particularly for presurgical evaluation of patients undergoing aortic root surgery, valve-sparing aortic surgery, or valve repair.
As no single parameter is adequate for determining AR severity, the grading of AR is carried out using a multiparametric approach [8,9]. Colour Doppler is critical for assessing the degree of regurgitation. Its major limitations include the presence of eccentric jets, diffuse jets, and jets originating along the entire coaptation line. A dense continuous wave signal reflects more regurgitant red blood cells. Pulse wave Doppler allows the evaluation of flow in the descending aorta from the suprasternal window and in the abdominal aorta. A brief diastolic flow reversal in the aorta is normal; however, the presence of holodiastolic flow reversal in the descending aorta is associated with severe AR. It is a simple and reliable index but, in older individuals who have a less compliant aorta, these measurements can be problematic and less definitive. Semi-quantitative (vena contracta [VC]) and quantitative (proximal isovelocity surface area [PISA]) are recommended in more than trivial regurgitation, although PISA quantitation of AR is used less often than in mitral regurgitation and it is impossible to measure it in a substantial proportion of patients. Jet deceleration rate (pressure half-time) is less used since it may be lengthened in chronic adaptation to severe AR. The regurgitant fraction calculated by the Doppler volumetric method is time-consuming and the potential for compounding multiple small measurement errors can lead to substantial overall inaccuracies.
Echocardiography is also essential in tracking the progressive increase in LV volume and the progressive worsening in its function due to the protracted LV volume overload. LV dilatation, particularly with preserved LV function, is a supportive sign of significant AR.
Conclusion
After publication of the latest guidelines, the essential or additional parameters are now accepted overall. These allow for the analysis of different AS scenarios due to various flow conditions and pressure gradients. A technical and clinical appraisal of echocardiography along with other imaging modalities can help to better understand the results and choose the right treatment. The evaluation of AR by Doppler echocardiography should be a comprehensive process, since each of the parameters used in this evaluation has advantages and limitations, as in AS. Vena contracta and flow reversal in the descending aorta seem to be the most robust indices. Other quantitative method can be proposed, but only to echocardiographers with extensive experience.



 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.