While genetic counseling is a critical step before undergoing genetic testing, it is important to understand that, it is not the end of the road once the DNA sample is collected. In fact, a significant part of genetic counseling occurs after the result is available. The aim is to provide personalized information to patients and their families, ensuring that everyone involved receives care tailored to their specific needs (1), as highlighted in the 2023 ESC Guidelines for Cardiomyopathies (2).
Understanding the Results: The Concept of Actionability
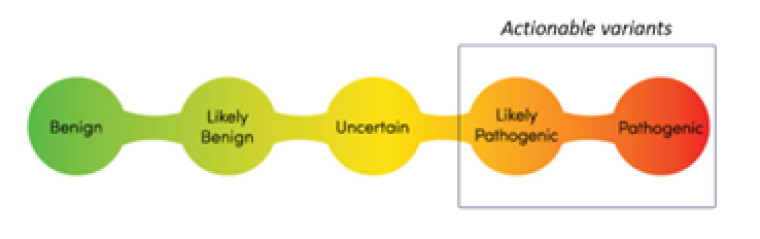
After sequencing, genetic variants are categorized into one of five groups, based on international guidelines formulated by the American College of Human Genetics. This classification helps to determine whether a variant is the cause of a given disease within a family. Developed by the American College of Medical Genetics, this system aids in interpreting these variants based on the frequency of the allele, the evidence in the literature, its association with similar phenotypes in other families, the predicted impact of the variant on protein function, as well as many other criteria (3). Variants range from benign or likely benign—suggesting they are not disease-causing, to variants of unknown significance, where there is not enough evidence for a definitive conclusion. The most clinically relevant categories are likely pathogenic or pathogenic variants, indicating strong evidence that these variants contribute to the disease. Variants in these latter categories are actionable, meaning they can guide decision-making in patient care, and can be used for clinical risk stratification as non-carriers can be reassured and discharged safely (4).
Communicating Results: The Challenge of Non-Conclusive Tests
One of the toughest tasks for genetic counselors is explaining to patients and their families that an inconclusive genetic test does not mean their condition is not hereditary. It is crucial to communicate that, even without a definitive genetic cause, relatives might still be at risk and should undergo periodic screening based on the family's identified conditions.
When Actionable Variants are Found: Guiding the Patient
The Importance of Cascade Genetic Testing
If an actionable variant is identified as causing the phenotype, cascade genetic testing is a priority to identify at-risk relatives who might benefit from specific drug avoidance recommendations, lifestyle modifications, and to identify cases with subclinical involvement. Cascade genetic testing usually starts with first-degree relatives including parents, siblings and descendants, although second-degree relatives might also benefit from screening in scenarios where a first-degree relative has died (2).
Conveying information about cascade genetic testing typically relies on the proband passing it on to the appropriate relatives, which might be challenging in some cases. Active facilitation by healthcare providers, including medical letters or direct contact with the proband’s permission, is crucial for a high turnout.
Genetic counseling often involves collaboration with a multidisciplinary team of healthcare professionals. This team may include genetic counselors, physicians, nurses, psychologists, and social workers, among others. By working together, healthcare providers can offer comprehensive care that addresses the medical, emotional, and social needs of patients and their families.
Avoiding Guilt
When discussing genetic conditions, it is important to navigate the emotional landscape with care. Many patients may irrationally blame themselves or feel guilty about passing a genetic variant to their offspring (6). It is essential to communicate that these conditions are the result of natural, random genetic variations beyond anyone's control. Genetic counselors play a vital role in providing emotional support (1).
Many patients and their families experience emotional distress when faced with genetic testing results. Providing access to support groups, counseling services, and coping strategies can help individuals navigate the emotional challenges associated with genetic conditions. Healthcare providers should offer holistic care that addresses both the medical and psychosocial needs of patients and their families (5).
Understanding Penetrance
Penetrance explains why not all individuals carrying a pathogenic genetic variant will exhibit the associated disease. It is a measure of the likelihood that a person carrying a specific genetic variant will show the phenotype or symptoms of the genetic condition. This variability can be influenced by multiple factors such as lifestyle, environment, and interactions with other genes. Educating patients about penetrance is crucial for setting realistic expectations about the risk of disease manifestation and for understanding the limitations of genetic testing. By grasping this concept, patients can better appreciate the nuances of genetic risk and the importance of regular health surveillance and lifestyle choices in influencing their overall health outcomes.
Reproductive Counseling
Finally, reproductive counseling is an essential component of genetic counseling, especially for younger carriers. It involves discussing the potential for passing on genetic conditions to future generations and exploring family planning options. This can include information on natural conception and its associated risks, the use of assisted reproductive technologies like IVF with preimplantation genetic testing (PGT) to reduce the likelihood of transmitting the condition, gamete donation and adoption. Reproductive counselling empowers individuals and couples to make informed decisions about their reproductive futures, considering their personal values, the specifics of their genetic condition, and the range of reproductive technologies and supports available.
Ongoing Research and Advances
As the field of genetics continues to evolve, ongoing research efforts and technological advances hold promise for improving genetic testing accuracy, accessibility, and treatment options. By staying informed about the latest developments in genetics, healthcare providers can better serve their patients and offer cutting-edge care that reflects the latest scientific advancements.
Useful links:
Genetic testing and counselling in the cardiomyopathies.
Presentation by Professor James Ware, during ESC Congress 2023

 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.